10 Common Methods for Medical Device Sterilization
Contaminated medical tools can lead to serious infections. That’s why any device that contacts sterile tissue or fluids, like surgical instruments or implants, must be completely free of microbes. The CDC classifies these as critical items, and sterilization is essential for patient safety. But not all devices can handle heat or moisture. Some are electronic, others are delicate or disposable. So, how do we sterilize them without damage?
In this article, we will break down the most common medical device sterilization methods, why they’re important, and how they differ, so you’ll know exactly which method suits which device and why. Let’s dive right in!
10 Different Sterilization Methods for Medical Devices
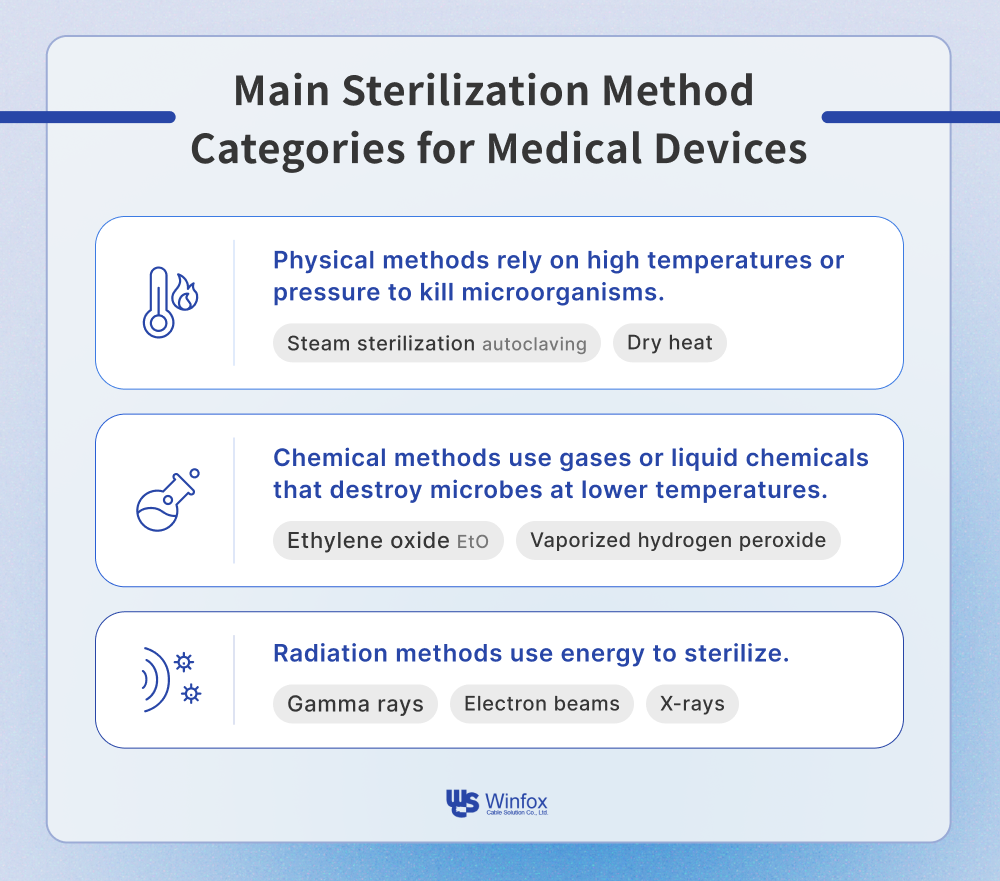
Most sterilization methods fall into three main categories: physical, chemical, and radiation-based. Each has its own strengths and ideal applications:
-
Physical methods rely on high temperatures or pressure to kill microorganisms. Think of steam sterilization (autoclaving) or dry heat.
-
Chemical methods use gases or liquid chemicals that destroy microbes at lower temperatures. Examples include ethylene oxide (EtO) and vaporized hydrogen peroxide.
-
Radiation methods use energy like gamma rays, electron beams, or X-rays to sterilize items without heat or moisture.
Here we’ll walk through some widely used sterilization methods, their pros and cons, and when to use each.
Steam Sterilization (Autoclaving)
Imagine locking your medical tools into a high-pressure cooker. That’s essentially how steam sterilization, or autoclaving, works. This method uses pressurized steam at around 121°C to destroy bacteria, viruses, and even hardy spores. The process takes place inside an autoclave, either a gravity displacement or high-speed pre-vacuum type, which allows steam to reach every crevice of the packaged device. Time, temperature, pressure, and steam quality are the key variables that determine the success of the process.
Steam sterilization is trusted around the world for a reason. It’s affordable, highly effective, and doesn’t leave behind toxic residues. Because steam can seep into fabrics and porous materials, it offers thorough sterilization with a wide safety margin. But not everything can handle the heat and moisture such as electronics, some plastics, and delicate biological materials can be damaged. Also, both the packaging and the device itself must be designed to allow proper steam flow, or sterility can’t be guaranteed. You’ll find steam sterilization in nearly every hospital and surgical center. It’s the go-to method for heat-stable items like surgical instruments, forceps, anesthesia equipment, implantables, and even pharmaceutical vials. When durability and simplicity matter, steam gets the job done.
Dry Heat Sterilization
Think of dry heat sterilization like baking your medical tools. Instead of using steam, it relies on hot air, typically at 160°C or higher, to oxidize and destroy microorganisms. Devices are placed in a dry heat oven and held at that temperature for an extended period. It’s slower than other methods, but for the right materials, it’s very effective.
Dry heat is ideal when moisture is the enemy. It’s perfect for items that would rust, corrode, or degrade if exposed to steam. The method is clean, non-toxic, and doesn't require special packaging. On the flip side, the high heat and long exposure time make it unsuitable for many modern medical devices. Only materials that can tolerate extended baking without warping or losing function can safely undergo this process. Dry heat sterilization is often used for glassware, metal tools, powders, and certain pharmaceuticals. It’s commonly employed in laboratories and manufacturing settings where high heat resistance is expected and needed.
Ethylene Oxide (Eto) Sterilization
Ethylene oxide sterilization is like sending a gas through every twist and turn of a device, targeting microbes in places heat or radiation can't reach. This method uses a highly reactive gas (EtO) to sterilize complex or heat-sensitive medical equipment. EtO works by altering the DNA and proteins of microorganisms, rendering them inactive. The process runs at low temperatures, typically below 60°C, and high humidity. For sterilization to be effective, the gas must thoroughly penetrate the device and remain in contact with all internal and external surfaces.
EtO is a workhorse for sterilizing modern medical devices, especially those made from plastics, resins, or electronics that can’t withstand high heat or moisture. It can handle items with intricate shapes, long lumens, and multilayer packaging. However, it's far from simple. EtO is toxic and flammable, so it must be handled with strict safety protocols. The process takes time, often up to a week, including gas exposure, aeration, and biological testing. Residual gas must also be monitored to ensure patient safety. EtO is the most widely used method in the US, responsible for sterilizing about half of all medical devices. It’s commonly used for syringes, IV sets, catheters, wound dressings, surgical kits, and any product with complex packaging or sensitive materials.
Vaporized Hydrogen Peroxide Sterilization (Low-Temperature/Glass Plasma Sterilization)
VHP sterilization is like a gentle fog that kills. It uses vaporized hydrogen peroxide, sometimes combined with plasma, to sterilize heat- and moisture-sensitive medical devices. The vapor spreads evenly across device surfaces and, in some systems, is energized into plasma to further enhance its microbe-killing power. Unlike older chemical methods, this one breaks down into harmless water and oxygen afterward.
This method is fast, clean, and highly effective for materials that can't handle traditional sterilization. It's also FDA-recognized as a well-established process, which simplifies the regulatory path for many device manufacturers. On the downside, VHP isn’t compatible with cellulosic materials like paper or cotton, and deep device channels can be hard to reach. Careful control of temperature, humidity, and gas flow is essential for consistent results.
VHP is commonly used to sterilize reusable surgical instruments, electronics, and heat-sensitive plastic devices. It’s especially valuable in hospital central sterilization departments and cleanroom settings.
Sporicidal Chemicals Sterilization
Instead of using heat or radiation, sporicidal chemical sterilization relies on powerful chemical agents, like peracetic acid or glutaraldehyde, to wipe out even the most resilient spores. Devices are soaked or flushed with these liquids for a set period, then thoroughly rinsed. It’s a hands-on method, ideal when other sterilization technologies can’t be applied.
This approach is ideal for instruments with narrow lumens or sensitive construction. Because it avoids heat and pressure, it’s especially useful for surgical scopes and endoscopes. However, it requires precision, both in handling strong chemicals and in validating that no residues remain. It’s not suitable for high-volume sterilization and demands careful rinsing and material compatibility. Used mostly in hospitals and clinics for high-level disinfection and sterilization of reusable, heat-sensitive tools like flexible endoscopes, surgical tubing, and components with internal channels.
Chlorine Dioxide Sterilization
Think of chlorine dioxide gas as a dry-cleaning solution for medical devices. It’s a powerful oxidizing agent that sterilizes at low temperatures, making it perfect for materials that can’t handle heat or moisture. Generated onsite, ClO₂ gas fills a sealed chamber and reacts with microbial cells, damaging their membranes and essential proteins.
Chlorine dioxide offers sterilization performance similar to vaporized hydrogen peroxide but with even better penetration into packaging. It operates at mild temperatures and is highly effective against spores. However, it requires tight environmental controls, including humidity and material compatibility. Corrugated boxes and cellulosic materials are not recommended, and materials must be oxidation-resistant.
This method is mostly used for sterilizing heat-sensitive items, including polymer-based tools, sealed containers, and devices with intricate packaging that require thorough gas exposure.
Ozone Sterilization
Ozone sterilization brings the power of nature into the sterilization suite. Ozone, a reactive form of oxygen, is generated on-site and introduced into a chamber at controlled humidity. It kills microbes by oxidizing their cell walls and internal components. Since it breaks down into oxygen after use, there are no chemical residues left behind.
This method is eco-friendly and operates at low temperatures, making it suitable for moisture- and heat-sensitive devices. It’s an excellent solution when environmental sustainability is a priority. That said, ozone is highly reactive and can damage certain materials, such as rubber or adhesives, so compatibility testing is essential. Ideal for sterilizing pre-packaged medical devices, including diagnostic kits, plastics, and electronics. It’s especially useful in smaller-scale, flexible production environments or where traditional methods aren't an option.
Gamma Irradiation Sterilization
Imagine a beam of invisible energy passing right through a box and killing every microorganism inside without even opening it. That’s the power of gamma irradiation. Using radioactive sources like cobalt-60, this method sends high-energy gamma rays into packaged medical devices, disrupting the DNA of microbes so they can’t reproduce or survive.
Gamma sterilization is incredibly effective for bulk processing. It’s fast, clean, and works well even with dense or layered packaging. Because it doesn’t rely on heat or pressure, it’s a good fit for many heat-sensitive devices. However, it’s not gentle on everything. Some materials, like PTFE and PVC, can degrade under gamma exposure, and sensitive biologics may not fare well. It also slightly increases product temperature, which needs to be factored into device design.
Gamma rays are used to sterilize everything from syringes and surgical gloves to implantables and diagnostic kits. In fact, nearly 40% of sterile medical devices in America are sterilized this way. It’s the backbone of many large-scale, single-use device production lines.
Electron Beam (E-Beam) Sterilization
Now, picture a laser-like stream of electrons fired at a packaged product, instantly destroying microbes on contact. That’s electron beam sterilization, or E-beam. It uses a concentrated beam of high-energy electrons to sterilize surfaces and shallow layers without raising the temperature too much. Unlike gamma rays, E-beam has a shallower penetration depth, but it’s highly targeted and fast.
E-beam is like gamma’s quick and gentle cousin. It’s better suited for materials that don’t tolerate gamma well and don’t rely on chemicals, steam, or high heat. Turnaround is ultra-fast, often under 8 hours, and it can be validated with straightforward bioburden testing. But because its penetration is limited, it’s not ideal for very thick or densely packed items. Also, packaging must be uniform to ensure consistent exposure.
E-beam is great for catheters, pre-filled syringes, tubing sets, and smaller devices that need a quick, low-impact sterilization method. It’s used less frequently than gamma but still sterilizes about 4.5% of devices in the country.
X-ray Sterilization
If gamma is like a sunbeam and E-beam like a laser pointer, X-ray sterilization sits somewhere in between. It uses high-energy photon radiation generated by accelerating electrons into a target. The resulting X-rays can pass through entire boxes or pallets of packaged medical devices, killing microorganisms by damaging their DNA and molecular structure.
These rays combine the deep penetration of gamma with some of the speed and flexibility of E-beam. They work well with dense or multilayer packaging, even if it’s not permeable. The process doesn’t involve vacuum cycles or high pressure, which is gentler on packaging seals. Still, the radiation can cause subtle changes in materials, like yellowing or crosslinking in plastics, which may impact product performance over time.
X-ray sterilization is gaining traction in sterilizing sealed medical kits, combination drug-device products, and complex packaging formats. It’s FDA-recognized and considered a valuable option when heat, moisture, or chemical sterilization isn’t viable.
| Method Name | Type | Material Compatibility | Key Features | Common Uses |
|---|---|---|---|---|
| Steam (Autoclaving) | Physical | Metals, heat-stable plastics | Affordable, reliable, no residue, uses high temp and moisture | Surgical tools, implants |
| Dry Heat | Physical | Glass, metals | Oxidizes microbes, high temperature, and long cycle time | Glassware, metal instruments |
| Ethylene Oxide (EtO) | Chemical | Plastics, electronics, complex devices | Penetrates complex designs, low temperature, long cycle, and potential residues | IV sets, catheters, surgical kits |
| Vaporized Hydrogen Peroxide | Chemical | Plastics, electronics | Low temp, clean, fast, no residue, FDA-recognized sterilization process | Reusable tools, electronics |
| Sporicidal Chemicals | Chemical | Scopes, reusable surgical items | Immersion/flush with strong chemicals requires rinsing | Endoscopes, surgical devices |
| Chlorine Dioxide (ClO₂) | Chemical | Polymers, sealed packs | Low temp, oxidizing gas, effective for heat-sensitive items | Heat-sensitive medical devices |
| Ozone | Chemical | Plastics, packaged items | Eco-friendly, low temp, strong oxidizing agent | Diagnostic kits, plastic devices |
| Gamma Irradiation | Radiation | Most materials (except PTFE, PVC) | Deep penetration, fast turnaround, validated by bioburden testing | Syringes, gloves, diagnostics |
| Electron Beam (E-Beam) | Radiation | Most plastics, surface sterilization | Quick cycle, minimal material impact, shallow penetration | Catheters, tubing |
| X-ray | Radiation | Sealed kits, dense packaging | Low dose, no vacuum needed, good for dense or multilayer packaging | Pre-packaged medical kits |
Common ISO Standards for Medical Device Sterilization
To protect patients and ensure the effectiveness of sterilization procedures, various ISO standards have been developed specifically for medical devices. These standards provide clear frameworks for validating, controlling, and monitoring sterilization methods. Below are some of the most widely used ISO standards in medical device sterilization.
ISO 17665 – Moist Heat Sterilization
ISO 17665, titled Sterilization of Health Care Products – Moist Heat, provides detailed guidance on how to develop, validate, and routinely control sterilization processes that use moist heat, such as steam autoclaving. The standard ensures that devices are consistently sterilized under defined conditions, reducing the risk of contamination. Originally released in 2006 and updated in 2009, ISO 17665 is currently undergoing further revision to align with modern practices. Steam sterilization service providers are expected to follow this standard to meet regulatory and quality expectations.
ISO 11135 – Ethylene Oxide (EtO) Sterilization
ANSI AAMI ISO 11135:2014 is a voluntary consensus standard that outlines how to properly use ethylene oxide (EtO) for sterilizing medical devices. According to the FDA, this standard describes in detail how to design, validate, and routinely monitor EtO sterilization processes to ensure both safety and effectiveness. It helps manufacturers create reliable sterilization protocols that meet regulatory requirements and reduce risks associated with EtO use.
ISO 10993-7 – EtO Residuals
ISO 10993-7:2008(R)2012 focuses specifically on the levels of residual ethylene oxide and its byproduct, ethylene chlorohydrin, that can remain on a medical device after sterilization. Since EtO is a known carcinogen, managing residual levels is critical for patient and worker safety. This standard provides limits for allowable residues and explains how to test for them. Following ISO 10993-7 helps ensure that sterilized devices are safe to handle and use, particularly when long-term or repeated exposure is a concern.
ISO 11137 – Radiation Sterilization
ISO 11137 governs the use of ionizing radiation, such as gamma rays or electron beams, to sterilize medical devices. The standard outlines procedures for dose setting, validation, and ongoing process control to confirm that the sterilization consistently meets microbial safety requirements. ISO 11137 is essential for manufacturers that rely on radiation as a non-thermal sterilization solution, especially for materials that are sensitive to heat or moisture.
ISO 22441 – Vaporized Hydrogen Peroxide (VH2O2) Sterilization
ISO 22441:2022 provides a standardized approach to developing and validating low-temperature sterilization processes using vaporized hydrogen peroxide (VH2O2). Recognized by the FDA, ISO 22441 designates VH2O2 as an Established Category A sterilization process, making it easier for manufacturers to meet 510(k) regulatory requirements. The FDA’s updated guidance for sterility in premarket submissions supports the use of this standard to improve efficiency and reduce regulatory burdens.

Why is It Important to Sterilize Medical Devices?
Sterilizing medical devices is essential to prevent infections that can arise from contaminated tools. Devices that come into contact with sterile tissues or fluids must be completely free of microorganisms. Failing to sterilize such instruments can lead to serious healthcare-associated infections, including surgical site infections and bloodstream infections.
Effective sterilization methods for medical devices play a direct role in protecting patient safety. When sterilization is performed correctly, hospitals see a significant drop in infection-related complications, which improves health outcomes and builds trust in healthcare services. Sterilization also ensures compliance with strict guidelines set by the CDC, FDA, WHO, and other health authorities. Healthcare providers must meet these requirements to avoid regulatory penalties and uphold care standards.
Sterilization safeguards healthcare workers as well. It prevents occupational exposure to infectious agents and harmful residues, particularly with methods like ethylene oxide, which has known health risks if mishandled. Using safer alternatives, such as vaporized hydrogen peroxide, helps protect both staff and the environment. Lastly, consistent sterilization helps prevent the spread of antibiotic-resistant bacteria in hospitals. Devices that aren’t properly sterilized can become carriers of dangerous pathogens, increasing the risk of outbreaks and complicating treatment.
Experience Excellence with Winfox Medical-Grade Cables
Proper sterilization of medical devices is more than a technical requirement. It’s essential for patient safety, infection control, regulatory compliance, and ensuring consistent device performance. Whether you're working with surgical tools, implants, or patient monitoring equipment, understanding different sterilization methods is key to selecting materials and components that can withstand repeated cycles without compromising function or safety.
That’s where Winfox comes in. As a trusted provider of medical-grade cables, Winfox offers fully customizable solutions engineered to meet various medical settings. With over 30 years of experience, we specialize in designing high-performance cables, such as ECG and patient monitoring cables, that combine durability, accuracy, and biocompatibility. From single-use to reusable designs, shielded cables, and from single to multi-conductor builds, our cables are developed to align with ISO 13485 and ISO 9001:2015 quality standards. To address the demands of different sterilization processes and end-use applications, we also provide plastic material solutions engineered to balance sterilization resistance with product performance. This ensures that every cable not only meets clinical requirements but also maintains functionality across its intended lifespan.
We offer no minimum order quantities, a broad selection of materials, and lead times as fast as 3 days. Whether your devices require resistance to heat, chemicals, or frequent disinfection, we have the expertise and production capabilities to deliver the custom cables that perform reliably in any clinical setting.
Contact us today for a quote or technical consultation, and let us support your next breakthrough in medical device design.